Why Design Thinking is Essential for Healthcare Innovation
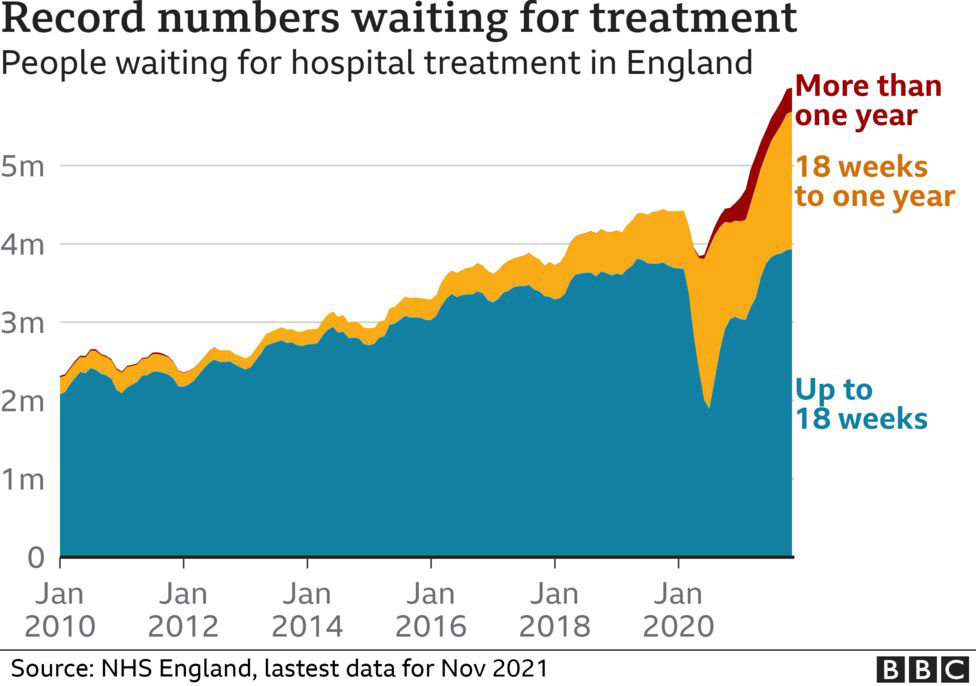
Healthcare Innovation is seen as an opportunity to solve our healthcare problems, but can it address these dramatically increasing challenges? Nowadays, everyone’s family on earth is feeling these challenges as they care about their and their beloved well-being. As healthcare systems try to improve their service, people live longer, and chronic diseases require more human and financial resources. Look at the hospital appointments. While the NHS in the UK mentioned that the waiting time for non-urgent treatments is 18 weeks, some appointments for chronic pain and other conditions can take months. Conditions that require close monitoring, such as thyroid function, got several delays because of the waiting time.
Related articles:
- Five Reasons to Utilise Patient-Centric Medical Innovation
- Design Thinking Tools and Methods Complete Guide
The video and online appointments were for a while, even before the COVID-19 pandemic. It was a solution for patients who wait long to visit doctors or have difficulties commuting to their doctors. However, the full implementation of digital health solution didn’t occur until the world went into s state of war against Covid-19. The technology has proven its effectiveness for two to three years despite the challenges. Thriva is another example of empowering patients through self-administered health technology. Patients can get their thyroid function tested through a home-based test where they get the results recorded through a mobile application. Home testing is still used widely to test people if they have Covid-19. The question is why health innovation solutions weren’t adopted as solutions when there was a need for them.
One of the significant problems that used to face GPs in the UK is the shallow appointments. Many of the patients don’t attend their appointments due to several reasons. Based on over 19 studies, the mean rate of missing appointments was around 12%. As a result, the waiting lists for attending doctor appointments increase dramatically, and the doctors and clinical resources are wasted because patients don’t show up. The Welsh NHS Betsi Cadwaladr University Health Board highlighted that the missed appointments in 2019/20 caused a total cost of £7.6m. These missed appointments cost the equivalent of 153 hospital beds, 166 nurses, 1,023 hip operations, 1,000 knee operations, and 7,058 cataract operations.
Recently, clinics adopted phone reminders to drive patients to attend the appointment. However, the idea of reminders was introduced many years before effectively applying it. Recent studies have reported the moderate to effective impact of phone reminders in improving appointment attendance rates.
New Ideas in the Healthcare Innovation
The obvious question that comes to mind is that if these solutions have been there for a long time, why are they not considered? When I discussed this problem with digital health experts and healthcare professionals, several reasons lay behind missing the adoption of technology happens during the design of the health product or service, such as:
1 – Healthcare innovation solutions are developed in an inter-disciplinary ecosystem, where collaborators from different backgrounds are involved in the interventions. These backgrounds vary from design, psychology, technology, engineering and others based on the final solution. Many healthcare organisations are entirely dominated by health and medical professionals, making it challenging to find solutions outside their expertise.
2 – Many of the health technology innovative solutions are not credible enough from the medical perspective to be deployed in action. At the same time, clinical trials are at the heart of evidence-based science. Healthcare innovation solutions don’t necessarily need to pass through clinical trials, which allows them to escape the trials’ costs and complex procedures (Check out: Why is Medical Technology Innovation so Hard?).
Why Design Thinking?
As highlighted in my previous article, Design Thinking Tools and Methods Complete Guide, design thinking shifts the traditional thinking mindset toward a human-centred one. In the meantime, the design thinking mindset encourages the team to think of technology and business parallel to the human-focused approach. The diagram below shows the balance between three main factors:
The patient needs: design extends this part to more than just the cure of the disease. It is about shifting patients’ experiences through service and product design. This focus involves usability, accessibility, form (how the product looks) and function (how it works). For example, the smart scale system allows patients to use their mobile app to follow up on their weight-related data daily by ensuring that their mobile is near the scale (Check out: Four Reasons to Expand Mobile Technology Usage in Medical Innovation).
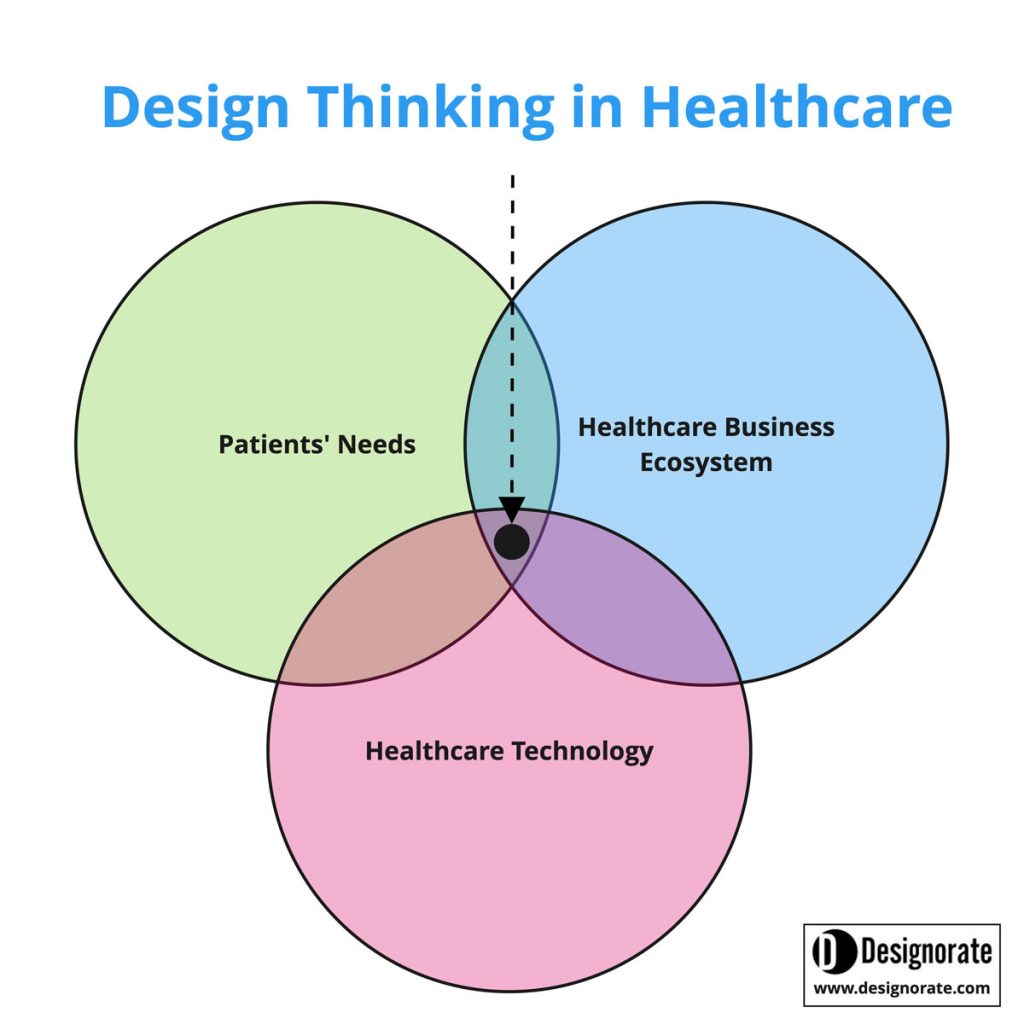
Business viability: without considering the business aspect of the healthcare innovation, it will not find the way toward market or hospital adoption. The new health technology should provide a financial advantage compared to its predecessors. For example, Noctura 400 mask is a non-invasive health technology for diabetic retinopathy (DR) patients or diabetic macular oedema (DMO). It replaces the traditional eye injection that could be repeated several times. Based on the National Institute of Health and Care Excellence (NICE), The total cost of conventional intravitreal anti-VEGF injections for DMO in 1 eye is £6,536 per patient per year. In contrast, the average annual cost for Noctura 400 mask per person ranges from £688 to £985 per person.
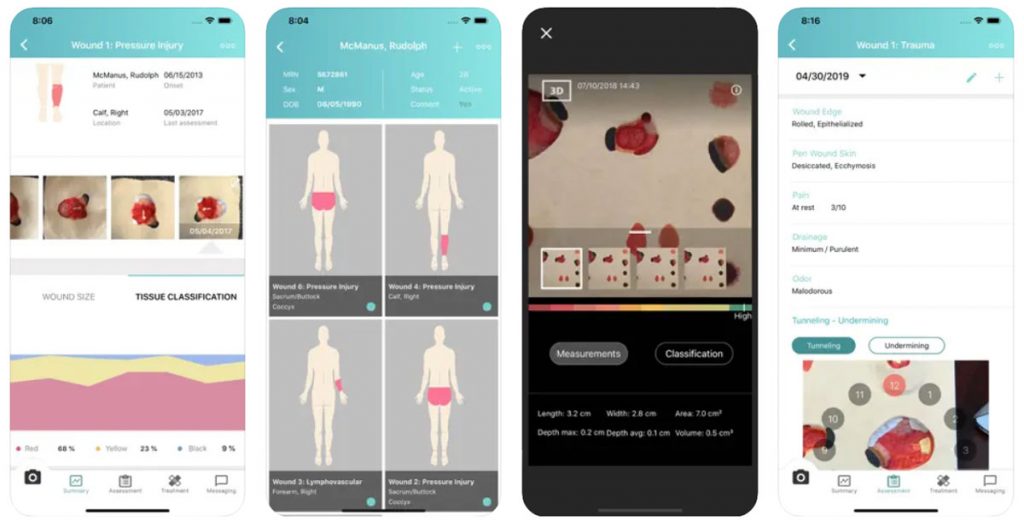
Technological feasibility: The central concept is that health solutions should be applicable from the technical and engineering perspective. The application extends to integrating the currently applied systems in health technology and digital health, especially in a hospital setup. An example of a technological application is eKare, a digital health app which enables patients to self-manage their wounds and foot ulcers while monitored remotely by their clinicians. Health technology such as eKara can reduce the number of hospital visits for ulcer checks, improve wound management, and reduce the risk of amputations.
In addition to the above three components, the design thinking process flows from the point before defining the project idea to the point after the final delivery. During this journey, several characteristics are included in the project, including the following:
Creativity and novelty of ideas: The primary starting point for the design thinking process is the exploring phase, where pictures are collected, analysed, and used to define the problem. At this stage, the team appreciates the nature of ambiguity and uncertainty to be able to explore different abstracted ideas (universes) and build a new connection between them. The squiggle shape by Newman presents a simple yet straightforward visualisation of the development of the design process.
Clear definition of the problem: The critical factor is to end up with a clear explanation of the problem that is based on field research, brainstorming, and root-cause analysis using tools such as 5 WHYs or the Cause Effect diagram.
Iteration and reflective practice: Testing the product with the end user and getting feedback is essential to improve the product based on feedback from the final user. User involvement and testing are primarily during the lean-nature design thinking process.
Conclusion
Design thinking uses a divergent approach to explore the different aspects of the situation or the problem, which provides an opportunity for more innovative healthcare solutions for patients and healthcare. Applying the design thinking process ensures the consideration of human, business, and technology factors. Furthermore, the usage of design practice encourages creativity and iteration in the development process.
The above examples are generic examples showing the benefits of healthcare innovation and digital health in improving patient service and how they can empower patients through self-administered solutions.
Bibliography
Aggarwal, A., Davies, J., & Sullivan, R. (2016). “Nudge” and the epidemic of missed appointments: can behavioural policies provide a solution for missed appointments in the health service?. Journal of Health Organization and Management.
Lorusso, L., Lee, J. H., & Worden, E. A. (2021). Design thinking for healthcare: transliterating the creative problem-solving method into architectural practice. HERD: Health Environments Research & Design Journal, 14(2), 16-29.
Parsons, J., Bryce, C., & Atherton, H. (2021). Which patients miss appointments with general practice and the reasons why: a systematic review. British Journal of General Practice, 71(707), e406-e412.
Roberts, J. P., Fisher, T. R., Trowbridge, M. J., & Bent, C. (2016, March). A design thinking framework for healthcare management and innovation. In Healthcare (Vol. 4, No. 1, pp. 11-14). Elsevier.
Brief Summary
Design thinking can be utilised to drive healthcare innovation and improve digital health. This adoption can be achieved by focusing on three main domains: patient needs and how to address them in products and services, the healthcare system ecosystem, and the adoption of healthcare technology such as digital health.
*Article image copyright: Hypertension vector created by pch.vector – www.freepik.com






